The Paper of the Month – September
21 Sep 2023Unveiling the value of estimating Stroke Outcomes after Endovascular Thrombectomy
Title: Unveiling the value of estimating Stroke Outcomes after Endovascular Thrombectomy
Author: Prof. Dr. Gustavo Saposnik – Editor-in-Chief, WSA
“It’s clear that policymakers and economists are going to be interested in the measurement of well-being primarily as it correlates with health; they also want to know whether researchers can validate subjective responses with physiological indices”.
– Daniel Kahneman (Professor of psychology, 2002 Nobel Prize Winner in Economic Science)
This article is a commentary on the following: Development and Validation of a Postprocedural Model to Predict Outcome After Endovascular Treatment for Ischemic Stroke, Vicky Chalos, MD,…..Hester F. Lingsma, PhD; JAMA Neurol. 2023;80(9):940-948. doi:10.1001/jamaneurol.2023.2392, https://jamanetwork.com/journals/jamaneurology/article-abstract/2807606 1
Summary of the findings:
The authors developed and validated a score (MR PREDICTS) to predict functional outcomes for individual patients with an ischemic stroke and a LVO in the anterior circulation who underwent endovascular thrombectomy (EVT) within 12 hours of symptom onset or last seen well.1
The score is based on the creation of a model from the Highly Effective Reperfusion Evaluated in Multiple Endovascular Stroke Trials (HERMES) collaboration and validated using data from the Dutch Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands (MR CLEAN) Registry.1,2 Participants included patients from different countries in Europe, North America, East Asia, and Oceania (derivation cohort), and multiple centers in the Netherlands (validation cohort).
A total of 781 patients (median [IQR] age, 67 [57-76] years; 414 men [53%]) constituted the validation cohort, and 3260 patients (median [IQR] age, 72 [61-80] years; 1684 men [52%]) composed the derivation cohort. Nine variables were included in the model: age, baseline National Institutes of Health Stroke Scale (NIHSS) score, prestroke mRS score, history of diabetes, occlusion location, collateral score, reperfusion grade, NIHSS score at 24 hours, and symptomatic intracranial hemorrhage 24 hours after EVT.
Overall, the models showed excellent discriminative ability for functional independence (C statistic, 0.91; 95% CI, 0.90-0.92) and survival (0.89; 95% CI, 0.88-0.90).
The authors concluded that MR PREDICTS can be applied after EVT to estimate functional outcomes for individual stroke patients with an LVO at 90 days.1
Commentary:
Prognostication is one of the most challenging tasks in medicine. Physicians face the difficult task of estimating outcomes when counselling patients and their families across multiple specialties.3 Stroke prognostication (e.g., short and long-term independency, risk of medical complications- infections, heart attack, venous thromboembolism, cognitive impairment, recovery of aphasia) is perhaps one of the most diverse predictions asked to stroke neurologists.3
Certainly, many prognostic scores were developed in the last two decades.4,5 Some scores included common clinical symptoms, vascular risk factors, pre-existing disability, stroke mechanism, and brain imaging data. Several studies applied those scores (e.g, iSCORE, THRIVE, ASTRAL, PLAN, SPAN-100) to their own cohorts, thus providing evidence of their performance across different ethnic populations.4,6-10
Although some of those scores (iSCORE, SPAN-100, DRAGON, SEDAN) were tested to estimate the response to thrombolysis (Alteplase)8,11-14, limited information was available regarding prognostication among stroke patients with an LVO undergoing EVT.15
In the present study,1 the authors created a model and then an online calculator (https://mdmtest.shinyapps.io/RRRR_2/) to facilitate the estimation of stroke outcomes.
What are the limitations of MR PREDICTS?
First, this score was created from a relatively small cohort of patients. For example, previous risk prognostic score models were derived from larger cohorts over 10,000 stroke patients (iSCORE, GWTG score) and following a similar design as the Framingham score.6,16,17
Second, some experts argue that scores created from smaller samples do not account for the wide variability affected by cluster of patients treated within the same institution, thus having less precise estimates.18,19 Some other known predictors of stroke outcomes (Atrial fibrillation, heart failure, cancer) were not included in the MR PREDICTS.6,20-24 This is not unexpected given the goal of having a parsimonious model when developing risk prognostic scores.
Third, the online calculator allow user to test different patient profile (Figures 1 and 2). However, it does not show whether differences between patients undergoing EVT vs. not receiving EVT are significant. The minimal clinically important difference was not reported.1
Finally, it is not clear how a patient with a pre-stroke disability (mRS=3) can reach a mRS 0-2 at 90 days with or without EVT.1
Despite these limitations, MR PREDICTS provides a practical estimation of stroke prognosis when comparing patients receiving and not receiving EVT when counselling patients and their family members. Furthermore, the treating physician can compare the likelihood of a favorable outcomes according to critical clinical variables.
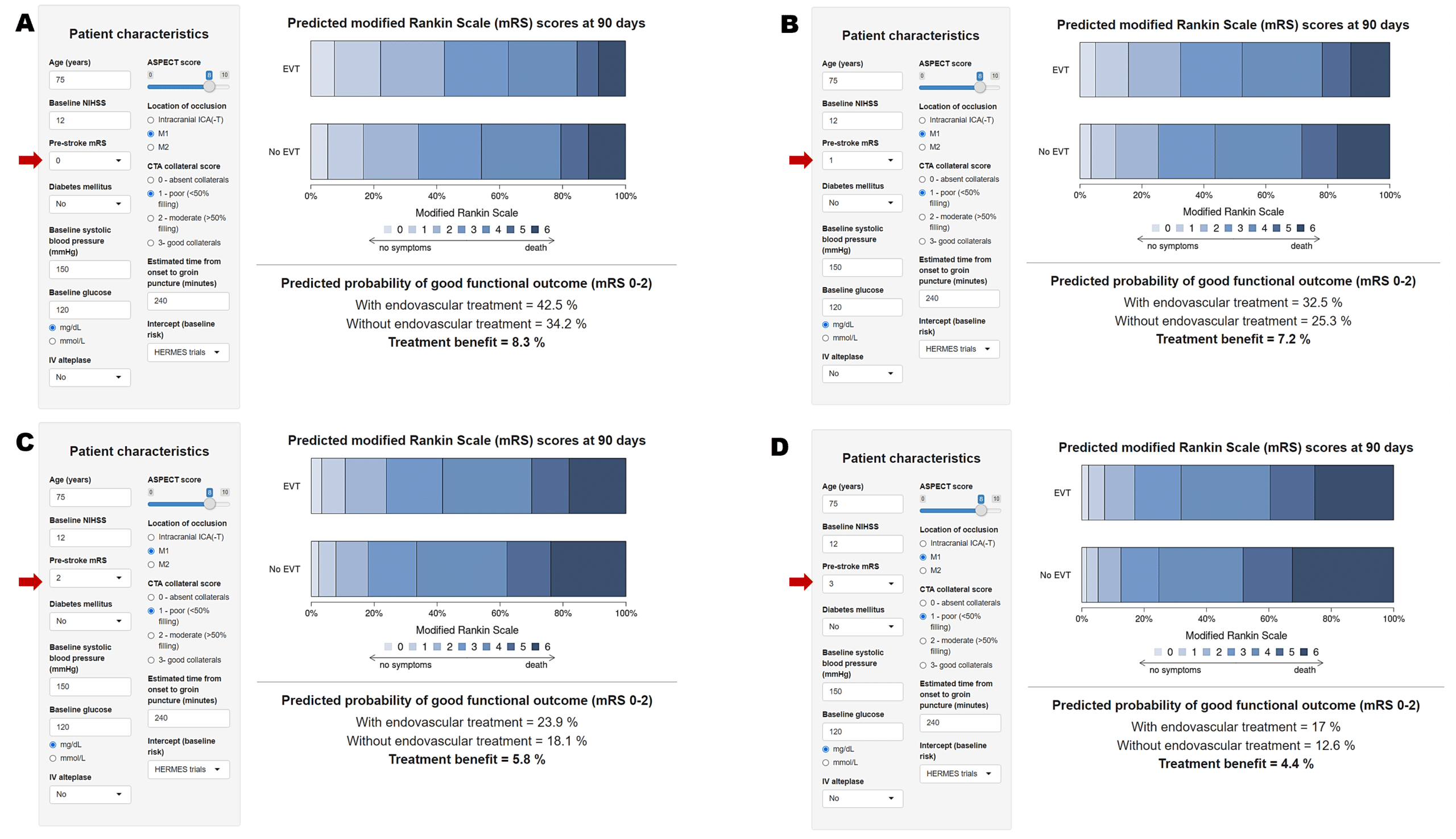
Figure 1.
Figure 2
Legends:
Figure 1– Predicted good functional outcome (mRS 0-2) with and without EVT for a 75 yo patient with a baseline NIHSS of 12, M1 occlusion, ASPECTS 8, and good CTA collateral score, not receiving tPA.
Panel A, B, C, and D represents the outcomes for a patient with a pre-stroke mRS=0, 1, 2, and 3, respectively. The red arrow indicates the pre-stroke mRS for the specific estimation. Treatment benefit between EVT vs. no EVT is in bold.
Note the decline in the expected benefit with EVT and no EVT by different pre-stroke mRS.
Figure 2– Predicted good functional outcome (mRS 0-2) with and without EVT for similar patient as represented in Figure 1, but with a poor collateral score (<50% filling). Panel A, B, C, and D represents the outcomes for a patient with a pre-stroke mRS=0, 1, 2, and 3, respectively. The red arrow indicates the pre-stroke mRS for the specific estimation. Treatment benefit between EVT vs. no EVT is in bold.
Note the decline in the expected benefit with EVT and no EVT by different pre-stroke mRS (and also when compared with estimations represented in Figure 1- showing good collateral flow. For example, the probability of a mRS 0-2 with EVT for scenario in Figure 1 with a pre-stroke mRS of 0 is 66.1%, whereas for similar patients with poor collateral flow and a pre-stroke disability of 3 is 17%).
Statistical differences were not available in the MR PREDICTS calculator.
References:
- Chalos V, Venema E, Mulder MJHL, Roozenbeek B, Steyerberg EW, Wermer MJH, Lycklama à Nijeholt GJ, van der Worp HB, Goyal M, Campbell BCV, et al. Development and Validation of a Postprocedural Model to Predict Outcome After Endovascular Treatment for Ischemic Stroke. JAMA Neurology. 2023;80:940-948. doi: 10.1001/jamaneurol.2023.2392
- Goyal M, Menon BK, van Zwam WH, Dippel DWJ, Mitchell PJ, Demchuk AM, Dávalos A, Majoie CBLM, van der Lugt A, de Miquel MA, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. The Lancet. 2016;387:1723-1731. doi: https://doi.org/10.1016/S0140-6736(16)00163-X
- Gao MM, Wang J, Saposnik G. The Art and Science of Stroke Outcome Prognostication. Stroke. 2020;51:1358-1360. doi: 10.1161/STROKEAHA.120.028980
- Kremers F, Venema E, Duvekot M, Yo L, Bokkers R, Nijeholt GLÀ, Es Av, Lugt Avd, Majoie C, Burke J, et al. Outcome Prediction Models for Endovascular Treatment of Ischemic Stroke: Systematic Review and External Validation. Stroke. 2022;53:825-836. doi: doi:10.1161/STROKEAHA.120.033445
- Matsumoto K, Nohara Y, Soejima H, Yonehara T, Nakashima N, Kamouchi M. Stroke Prognostic Scores and Data-Driven Prediction of Clinical Outcomes After Acute Ischemic Stroke. Stroke. 2020;51:1477-1483. doi: doi:10.1161/STROKEAHA.119.027300
- Saposnik G, Kapral MK, Liu Y, Hall R, O’Donnell M, Raptis S, Tu JV, Mamdani M, Austin PC, Investigators of the Registry of the Canadian Stroke N, et al. IScore: a risk score to predict death early after hospitalization for an acute ischemic stroke. Circulation. 2011;123:739-749. doi: 10.1161/CIRCULATIONAHA.110.983353
- Saposnik G, Raptis S, Kapral MK, Liu Y, Tu JV, Mamdani M, Austin PC, Investigators of the Registry of the Canadian Stroke N, the Stroke Outcome Research Canada Working G. The iScore predicts poor functional outcomes early after hospitalization for an acute ischemic stroke. Stroke. 2011;42:3421-3428. doi: 10.1161/STROKEAHA.111.623116
- Park TH, Park SS, Ko Y, Lee SJ, Lee KB, Lee J, Kang K, Park JM, Choi JC, Kim DE, et al. The iScore predicts clinical response to tissue plasminogen activator in Korean stroke patients. J Stroke Cerebrovasc Dis. 2014;23:367-373. doi: 10.1016/j.jstrokecerebrovasdis.2013.05.025
- Xu J, Tao Y, Xie X, Liu G, Wang A, Wang Y, Wang Y. A Comparison of Mortality Prognostic Scores in Ischemic Stroke Patients. J Stroke Cerebrovasc Dis. 2016;25:241-247. doi: 10.1016/j.jstrokecerebrovasdis.2015.09.021
- Pan Y, Peng Y, Chen W, Wang Y, Lin Y, He Y, Wang N, Wang Y. THRIVE-c score predicts clinical outcomes in Chinese patients after thrombolysis. Brain Behav. 2018;8:e00927. doi: 10.1002/brb3.927
- Cooray C, Mazya M, Bottai M, Dorado L, Skoda O, Toni D, Ford GA, Wahlgren N, Ahmed N. External Validation of the ASTRAL and DRAGON Scores for Prediction of Functional Outcome in Stroke. Stroke. 2016;47:1493-1499. doi: 10.1161/STROKEAHA.116.012802
- Strbian D, Meretoja A, Ahlhelm FJ, Pitkaniemi J, Lyrer P, Kaste M, Engelter S, Tatlisumak T. Predicting outcome of IV thrombolysis-treated ischemic stroke patients: the DRAGON score. Neurology. 2012;78:427-432. doi: 10.1212/WNL.0b013e318245d2a9
- Saposnik G, Reeves MJ, Johnston SC, Bath PM, Ovbiagele B, Collaboration V. Predicting clinical outcomes after thrombolysis using the iScore: results from the Virtual International Stroke Trials Archive. Stroke. 2013;44:2755-2759. doi: 10.1161/STROKEAHA.113.001343
- Saposnik G, Fang J, Kapral MK, Tu JV, Mamdani M, Austin P, Johnston SC, Investigators of the Registry of the Canadian Stroke N, Stroke Outcomes Research Canada Working G. The iScore predicts effectiveness of thrombolytic therapy for acute ischemic stroke. Stroke. 2012;43:1315-1322. doi: 10.1161/STROKEAHA.111.646265
- Ben Hassen W, Raynaud N, Bricout N, Boulouis G, Legrand L, Ferrigno M, Kazemi A, Bretzner M, Soize S, Farhat W, et al. MT-DRAGON score for outcome prediction in acute ischemic stroke treated by mechanical thrombectomy within 8 hours. J Neurointerv Surg. 2020;12:246-251. doi: 10.1136/neurintsurg-2019-015105
- Smith EE, Shobha N, Dai D, Olson DM, Reeves MJ, Saver JL, Hernandez AF, Peterson ED, Fonarow GC, Schwamm LH. Risk Score for In-Hospital Ischemic Stroke Mortality Derived and Validated Within the Get With The Guidelines–Stroke Program. Circulation. 2010;122:1496-1504. doi: doi:10.1161/CIRCULATIONAHA.109.932822
- Sullivan LM, Massaro JM, D’Agostino Sr. RB. Presentation of multivariate data for clinical use: The Framingham Study risk score functions. Statistics in Medicine. 2004;23:1631-1660. doi: https://doi.org/10.1002/sim.1742
- Concato J, Feinstein AR, Holford TR. The risk of determining risk with multivariable models. Ann Intern Med. 1993;118:201-210. doi: 10.7326/0003-4819-118-3-199302010-00009
- Cook NR. Use and Misuse of the Receiver Operating Characteristic Curve in Risk Prediction. Circulation. 2007;115:928-935. doi: doi:10.1161/CIRCULATIONAHA.106.672402
- Pana TA, Mohamed MO, Mamas MA, Myint PK. Prognosis of Acute Ischaemic Stroke Patients with Cancer: A National Inpatient Sample Study. Cancers (Basel). 2021;13. doi: 10.3390/cancers13092193
- Lin H-J, Wolf PA, Kelly-Hayes M, Beiser AS, Kase CS, Benjamin EJ, D’Agostino RB. Stroke Severity in Atrial Fibrillation. Stroke. 1996;27:1760-1764. doi: doi:10.1161/01.STR.27.10.1760
- Saposnik G, Gladstone D, Raptis R, Zhou L, Hart RG, Investigators of the Registry of the Canadian Stroke N, the Stroke Outcomes Research Canada Working G. Atrial fibrillation in ischemic stroke: predicting response to thrombolysis and clinical outcomes. Stroke. 2013;44:99-104. doi: 10.1161/strokeaha.112.676551
- Pongmoragot J, Lee DS, Park TH, Fang J, Austin PC, Saposnik G. Stroke and Heart Failure: Clinical Features, Access to Care, and Outcomes. Journal of Stroke and Cerebrovascular Diseases. 2016;25:1048-1056. doi: https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.01.013
- Li D, Wang Y, Ze F, Zhou X, Li X-B. Risk Predictors of 3-Month and 1-Year Outcomes in Heart Failure Patients with Prior Ischemic Stroke. Journal of Clinical Medicine. 2022;11:5922.
Interview to Author Dr. Vicky Chalos-Andreou:
1. What did you set out to study?
We developed and externally validated a prediction model for individual patients who underwent endovascular treatment (EVT) for ischemic stroke. This model may be used by treating physicians the day after EVT to predict outcome after 3 months. It is a prognostication tool only and does not serve to identify patients who may benefit from EVT.
2. Why this topic?
After EVT was introduced in clinical practice, we noticed that patients, family members, but also treating physicians, were very often wondering to what extent the patient will recover; Will the patient become functionally dependent again? Will the patient survive? As it was not easy to answer these questions for individual patients, because these outcomes depend on multiple factors and are highly variable, we agreed a probabilistic prediction model was needed. However, we noticed that most existing prediction models of EVT were serving to identify patients who may benefit from EVT, which means that post-procedural data – which can improve outcome prediction – were not included in the model. Existing post-procedural models were derived from cohorts of patients treated before the landmark trials, had methodological shortcomings, lacked validation, or had a different purpose. Therefore we decided to develop and validate a new model intended for the purpose of prognostication after EVT only.
3. What were the key findings?
We found that the combination of 9 routinely available pre-procedural and post-procedural characteristics can be used within one day, at or around 24 hours after EVT to accurately predict functional outcome. External validation model showed excellent discriminative ability for both functional independence (mRS 0-2: 0.91) and survival (mRS 0-5: 0.89) and good calibration, after which the model was further optimized through updating for use in contemporary clinical practice.
4. Why is it important? Or how might these results impact clinical practice?
This model – for which we developed an online calculator – may already be used in clinical practice by neurologists, stroke physicians, and rehabilitation specialists as a contemporary tool to aid in predicting outcome of individual patients that underwent EVT. It may result in more homogeneous outcome predictions across different physicians, and may guide these physicians in adapting and personalizing their patient’s follow-up and rehabilitation plans.
5. What surprised you most?
Although we expected NIHSS to be a major predictor of functional outcome – which is why we had also decided to develop a model of NIHSS at 24h alone – we were surprised by the fact that 8 additional characteristics, not only age, baseline NIHSS and NIHSS after 24h, but also diabetes mellitus, occlusion location, eTICI, CTA-collateral score and symptomatic ICH could be included in the model, and thus one by one also improved outcome prediction.
6. What’s next for this research?
Now that EVT becomes more widely available throughout the world and for larger patient populations as the selection criteria for EVT broaden, the model needs to be further externally validated in different patient populations and then updated, so that predictions will still be up to date for contemporary patients. As for us, we would first like to validate the model for patients who underwent EVT 24 hours symptom onset.
7. Is there anything you’d like to add?
This work is an extension of previous work, that resulted in MR PREDICTS, the prediction model for prediction of outcome and benefit after EVT within 6h for ischemic stroke. We hope to further expand and validate these models to make them applicable to the broad range of indications for EVT that is developing now.