The Paper of The Month – February
08 Feb 2023Title: CEA or CAS in asymptomatic carotid stenosis?
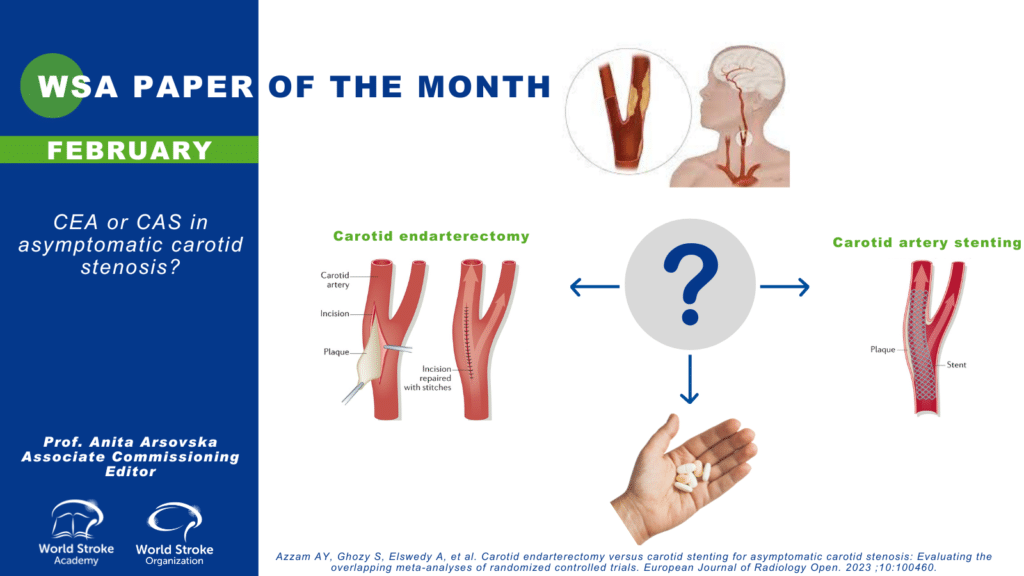
Title: CEA or CAS in asymptomatic carotid stenosis?
Author: Prof. Dr. Anita Arsovska – WSA Associate Commissioning Editor
This article is a commentary on the following: Azzam AY, Ghozy S, Elswedy A, et al. Carotid endarterectomy versus carotid stenting for asymptomatic carotid stenosis: Evaluating the overlapping meta-analyses of randomized controlled trials. European Journal of Radiology Open. 2023 ;10:100460.
Summary of the findings
Management of asymptomatic carotid stenosis (ACS) ranges from open surgical approaches, minimally invasive endovascular interventions, and medical therapeutics. Comparison of these interventions has been inconsistent and non-comprehensive. The authors did a comparison of 5 published meta-analyses that compared carotid endarterectomy (CEA) and carotid stenting (CAS) in ACS patients (1). They found that CEA reduced the rate of ischemic stroke and stroke-related mortality. On the other hand, CAS led to a lower rate of intraoperative cranial nerve injury. There was no significant difference between CEA and CAS in ipsilateral stroke and myocardial infarction events.
Commentary
ACS is defined as the presence of atherosclerotic narrowing of the proximal internal carotid artery by ≥50% at the level of bifurcation in individuals with no history of recent (within the last six months) ischemic stroke/TIA involving ipsilateral carotid territory (2). Stenosis of 50%–69% is regarded as moderate degree, while stenosis ≥70% is generally considered as severe degree (3). However, there are inconsistencies between definitions of severity in ACS and symptomatic stenosis, which also vary among studies depending on the method used for assessment of stenosis (4). Some criteria also use >60% definition.
Guidelines recommendations regarding the management of ACS
Guidelines by the European Society of Vascular Surgery, European Society for Cardiology and American Heart and Stroke Association suggest that CEA or CAS should be considered for patients with ACS (60%–99%) at average surgical risk, provided the documented perioperative stroke/death rate is less than 3% and the patient’s life expectancy exceeds 5 years (5, 6, 7, 8) Although all the guidelines suggest forming a multidisciplinary team for the management of these patients, the recommendations are not clear when it comes to CAS in both patients at average risk and high risk of complications of CEA (4). ESO guidelines (2021) that are based on moderate quality evidence, recommend CEA in patients with ≥60–99% asymptomatic carotid stenosis considered to be at increased risk of stroke on best medical treatment (BMT) alone. Based on a very low quality evidence, ESO recommends against CAS as a routine alternative in patients with asymptomatic carotid stenosis compared to best medical therapy alone (9).
CREST-2 trial- Carotid revascularization for primary prevention of stroke (CREST-2) is two independent multicenter, randomized controlled trials of carotid revascularization and intensive medical management versus medical management alone in patients with asymptomatic high-grade carotid stenosis (10). One trial will randomize patients in a 1:1 ratio to CEA versus no CEA and another will randomize patients in a 1:1 ratio to CAS with embolic protection versus no CAS. Medical management will be uniform for all randomized treatment groups. Estimated enrollment is 2480 participants and estimated study completion date is February 2026.
Lal B et al. reported the periprocedural outcomes in a cohort of CAS performed for asymptomatic and symptomatic carotid stenosis (11). CAS was performed by experienced operators using appropriate patient selection and optimal technique. In that setting, a broad group of interventionists achieved very low periprocedural stroke and death (S/D) rates for asymptomatic and symptomatic patients (the 30-day rate of S/D was 1.4% for asymptomatic, 2.8% for symptomatic, and 2.0% for all patients).
The 2nd European Carotid Surgery Trial (ECST-2) is a randomised clinical trial comparing immediate revascularisation versus optimised medical therapy alone in patients with symptomatic and asymptomatic carotid stenosis at low to intermediate risk of stroke. It will provide new data on the efficacy of modern optimal medical therapy alone versus added carotid revascularisation in patients with carotid stenosis at low to intermediate risk of future stroke selected by individualised risk assessment (12). The authors anticipate that the results of baseline brain and carotid plaque MRI will provide data to improve the prediction of the risk of stroke and the effect of treatment in patients with carotid stenosis.
Conclusion
We need further studies that would investigate the safety and efficacy of CAS versus CAS in order to recommend the best therapeutic approach in ACS.
References
- Azzam AY, Ghozy S, Elswedy A, et al. Carotid endarterectomy versus carotid stenting for asymptomatic carotid stenosis: Evaluating the overlapping meta-analyses of randomized controlled trials. European Journal of Radiology Open. 2023 ;10:100460.
- den Hartog AG, Achterberg S, Moll FL, Kappelle LJ, Visseren FL, van der Graaf Y, et al Asymptomatic carotid artery stenosis and the risk of ischemic stroke according to subtype in patients with clinical manifest arterial disease Stroke. 2013;44:1002–7
- Chatzikonstantinou A, Wolf ME, Schaefer A, Hennerici MG. Asymptomatic and symptomatic carotid stenosis: An obsolete classification?? Stroke Res Treat. 2012;2012:340798
- Sudheer P, Vibha D, Misra S. Asymptomatic Carotid Stenosis: Several Guidelines with Unclear Answers. Ann Indian Acad Neurol. 2022 Mar-Apr;25(2):171-176.
- Eckstein HH. European Society for Vascular Surgery guidelines on the management of atherosclerotic carotid and vertebral artery disease. Eur J Vasc Endovasc Surg. 2018;55:1–2.
- Aboyans V, Ricco JB, Bartelink MEL, Björck M, Brodmann M, Cohnert T, et al. 2017 ESC guidelines on the diagnosis and treatment of peripheral arterial diseases, in collaboration with the European Society for Vascular Surgery (ESVS): Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteriesEndorsed by: The European Stroke Organization (ESO) The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS) Eur Heart J. 2018;39:763–816.
- Ricotta JJ, Aburahma A, Ascher E, Eskandari M, Faries P, Lal BK, et al. Updated Society for Vascular Surgery guidelines for management of extracranial carotid disease: Executive summary. J Vasc Surg. 2011;54:832–6.
- Goldstein LB, Bushnell CD, Adams RJ, Appel LJ, Braun LT, Chaturvedi S, et al. Guidelines for the primary prevention of stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. 2011;42:517–84.
- Bonati LH, Kakkos S, Berkefeld J, et al. European Stroke Organisation guideline on endarterectomy and stenting for carotid artery stenosis. European Stroke Journal. 2021;6(2):I-XLVII.
- https://clinicaltrials.gov/ct2/show/NCT02089217
- Lal BK, Roubin GS, Rosenfeld K, et al. Quality assurance for carotid stenting in the CREST-2 Registry. J Am Coll Cardiol. 2019;74:3071-3079.
- Cheng SF, van Velzen TJ, Gregson J. et al. The 2nd European Carotid Surgery Trial (ECST-2): rationale and protocol for a randomised clinical trial comparing immediate revascularisation versus optimised medical therapy alone in patients with symptomatic and asymptomatic carotid stenosis at low to intermediate risk of stroke. 2022; Trials 23, 606.