The Paper of the Month August
01 Aug 2022Title: Recent advances in posterior circulation stroke management
Title: Recent advances in posterior circulation stroke management
Author: Prof. Anita Arsovska, Associate Commissioning Editor WSA
This article is a commentary on the following
Commentary
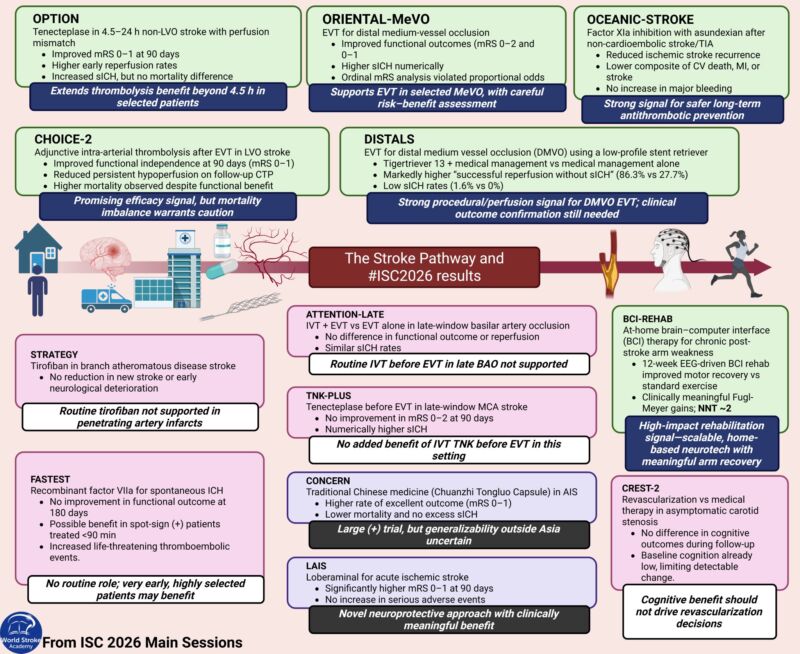
Summary of findings:The authors conducted a literature search on Pubmed on posterior circulation stroke acute management/secondary prevention and highlighted recent advances (1). Intravenous thrombolysis has similar benefits and lower risk of haemorrhage than in the anterior circulation.The benefits of mechanical thrombectomy extends to the BA occlusion, but the effects in other arteries of the posterior circulation stream remain uncertain. Decompressive craniectomy is recommended in ischaemic and haemorrhagic space-occupying cerebellar strokes. Secondary prevention includes aggressive treatment of cerebrovascular risk factors and short term dual antiplatelet therapy. For symptomatic basilar and intracranial vertebral stenosis, medical therapy is the preferred option over stenting. For symptomatic extracranial vertebral stenosis, stenting is an option particularly for recurrent events.
Discussion
Posterior circulation stroke accounts for 5-10% of ischaemic strokes (2).Compared to anterior circulation strokes, posterior strokes are characterized by a greater complexity of clinical symptoms, greater unpredictability of the disease’s course, and clinical variability. Symptoms often include dizziness, diplopia, dysarthria, dysphagia, disequilibrium, ataxia, visual field deficits and “crossed” deficits (cranial nerve territory symptoms on one side and sensory or motor deficits of the opposite arm and leg). The site of the occlusion has been associated with the underlying mechanism (e.g. PCA stroke are more commonly related to embolic or in-situ atherosclerotic disease).
Current guidelines for stroke treatment and prevention do not specifically address the issue of anterior vs posterior stroke management. They mostly focus on the anterior circulation.
ESO guidelines (2021) for the use of short-term dual antiplatelet therapy early after minor stroke and high-risk TIA make a strong recommendation based on high quality of evidence for use of 21-days of dual antiplatelet therapy with aspirin and clopidogrel in people with a non-cardioembolic minor ischaemic stroke or high-risk TIA in the past 24 hours (3). They make a weak recommendation based on moderate quality evidence for 30-days of dual antiplatelet therapy with aspirin and ticagrelor in people with non-cardioembolic mild to moderate ischaemic stroke or high-risk TIA in the past 24 hours.The new ESO guidelines (2022) confirm again that dual antiplatelet therapy with aspirin and clopidogrel after the first 90 days should be avoided (4). Latest ESO guidelines (2022) regarding management of intracranial atherosclerotic disease (ICAD) provided no evidence-based recommendations regarding the optimal detection strategy and management of asymptomatic ICAD, however in symptomatic ICAD, moderate-level evidence was found to recommend against the use of oral anticoagulation as preferred antithrombotic drug, in favor of antiplatelets (5). Low-level evidence recommended in favor of double antiplatelet as the antithrombotic treatment of choice in symptomatic ICAD patients, for a duration of 90 days. Endovascular therapy with intracranial angioplasty and/or stenting was not recommended as a treatment of first choice in high-grade symptomatic ICAD. Regarding neurosurgical interventions, the available evidence does not support their use as front line therapies in patients with high-grade ICAD (table 1).
Table 1. Current treatment options for posterior circulation
| Intravenous thrombolysis | Endovascular treatment | Intraarterial thrombolysis | Antiplatelets | Anticoagulants | Surgical treatment | |
| ICAD | √ | X | X | √ | X | X |
| SVD | √ | X | X | √ | X | X |
| LAD | √ | √ | X | √ | X | √ |
| Cardiogenic/
embolic |
√ | X | X | X | √ | X |
| Undetermined | √ | X | X | √ | X | X |
Abbreviations: ICAD- intracranial atherosclerotic disease; SVD- small vessel disease; LAD- large artery disease.
√- existing evidence
X – no evidence
Keylearningpoints (1):
- Thrombolysis for posterior circulation stroke appears to have similar benefit for the anterior circulation. The International Stroke Trial-3 was one of the only IVT RCT where the site of stroke was recorded; the authors observed that the risks and benefits of stroke thrombolysis were consistent across a wide range of patient characteristics with no clearly significant (P<0.01) interactions between r-tPA and baseline clinical characteristics (6).
- EVT is effective in BAO patients. Further RCTs are required to determine effectiveness in PCA and VA occlusions.
- Decompressive surgery may be needed for posterior fossa infarction and hemorrhage (hematoma larger than 3 cm, obstruction of the quadrigeminal cistern, and compression of the fourth ventricleare surgical criteria).
- The recurrent stroke risk after a posterior circulation TIA and/or a minor stroke issimilar to the anterior circulation, with highest incident risk for large artery
- For symptomatic basilar and intracranial vertebral stenosis, medical therapy is the recommended option over stenting.
- For symptomatic extracranial vertebral stenosis, stenting is a reasonable alternative for recurrent events (in cases with failure of medical management). Medical therapy is the recommended option for initial presentation. More data from clinical trials is required comparing its efficacy with best medical therapy.
Conclusion
Limited evidence-based information is available regarding the benefits and treatment for posterior circulation strokes. Most evidence is coming from ICAD studies (comparing intervention- stenting/angioplasty vs medical treatment). We need to learn more about the differential treatment effect by stroke mechanism of antithrombotics, anticoagulants and other interventional modalities for stroke prevention in the posterior circulation.
References
- Markus HS, Michel P. Treatment of posterior circulation stroke: acute management and secondary prevention. Int J Stroke. 2022 Jun 6:17474930221107500. doi: 10.1177/17474930221107500.
- Werring D. Posterior circulation ischaemic stroke BMJ 2014; 348 :g3175 doi:10.1136/bmj.g3175.
- Dawson J et al.European Stroke Organisation expedited recommendation for the use of short-term dual antiplatelet therapy early after minor stroke and high-risk TIA. European Stroke Journal. 2021;6(2):CLXXXVII-CXCI. doi:1177/23969873211000877
- Dawson J et al. European Stroke Organisation (ESO) guideline on pharmacological interventions for long-term secondary prevention after ischaemic stroke or transient ischaemic attack. European Stroke Organisation 2022. European Stroke Journal I–XLI, doi10.1177/23969873221100032.
- Psychogios M, Brehm A, López-Cancio E, et al. European Stroke Organisation guidelines on treatment of patients with intracranial atherosclerotic disease. European Stroke Journal. June 2022. doi:1177/23969873221099715
- Lindley, RI, Wardlaw, JM, Whiteley, WN, et al. Alteplase for acute ischemic stroke: outcomes by clinically important subgroups in the Third International Stroke Trial. Stroke 2015; 46: 746–756.
Video Interview